Page Outline
- Introduction
- The Humoral Response Begins with Phagocytosis at the Infection Site
- Phagocytes Present Antigen to Helper T Cells
- Helper T Cells Activate B Cells
- Interactive Table: The Humoral Response
- Antibodies Help Neutralize Pathogens in a Variety of Ways
- Quiz: The Humoral System
1. Introduction
The specific immune response involves three steps:
- Recognition: identifying and communicating about surface molecules on the invading pathogen.
- Overcoming: unleashing specialized proteins (antibodies) and cells (killer T cells) that defeat the pathogen.
- Remembering: creating memory cells that enable you beat back repeat infections by the same pathogen.
In the previous tutorial, we explored the basis of recognition. Here’s a quick summary.
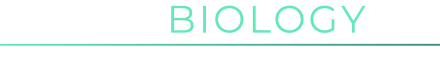
B and T cells are covered with receptors (only a few of which are shown in the diagram to your left, at “1”). Due to recombination and mutation of genes for receptors, we wind up with a vast army of genetically distinct B and T cells, each with uniquely shaped antigen binding sites.
In this tutorial, we’ll look at how B cells are activated to release antibodies, a response that’s called humoral immunity. Let’s go.
2. The humoral response begins with phagocytosis at the infection site
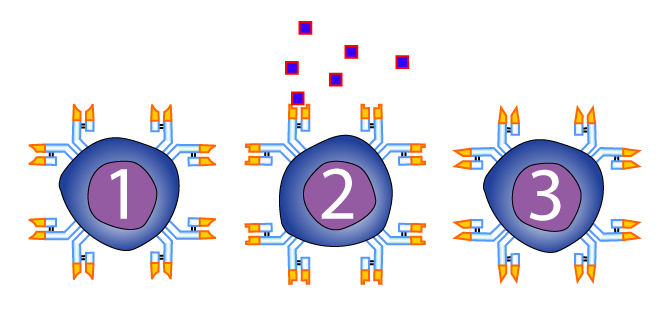
 In the first tutorial in this series, I explained how a key part of the non-specific immune response was phagocytosis. During phagocytosis, our neutrophils, macrophages, and dendritic cells (represented at left by “2”) attack invading pathogens (“1”) and swallow them up.
In the first tutorial in this series, I explained how a key part of the non-specific immune response was phagocytosis. During phagocytosis, our neutrophils, macrophages, and dendritic cells (represented at left by “2”) attack invading pathogens (“1”) and swallow them up.
For some phagocytic cells, that’s the end of their contribution to the immune response. But for other phagocytes, phagocytosis is just the first part of their job. Their next move is to relay the information about what they’ve engulfed to the specific immune response, so that weapons like antibodies can be unleashed.
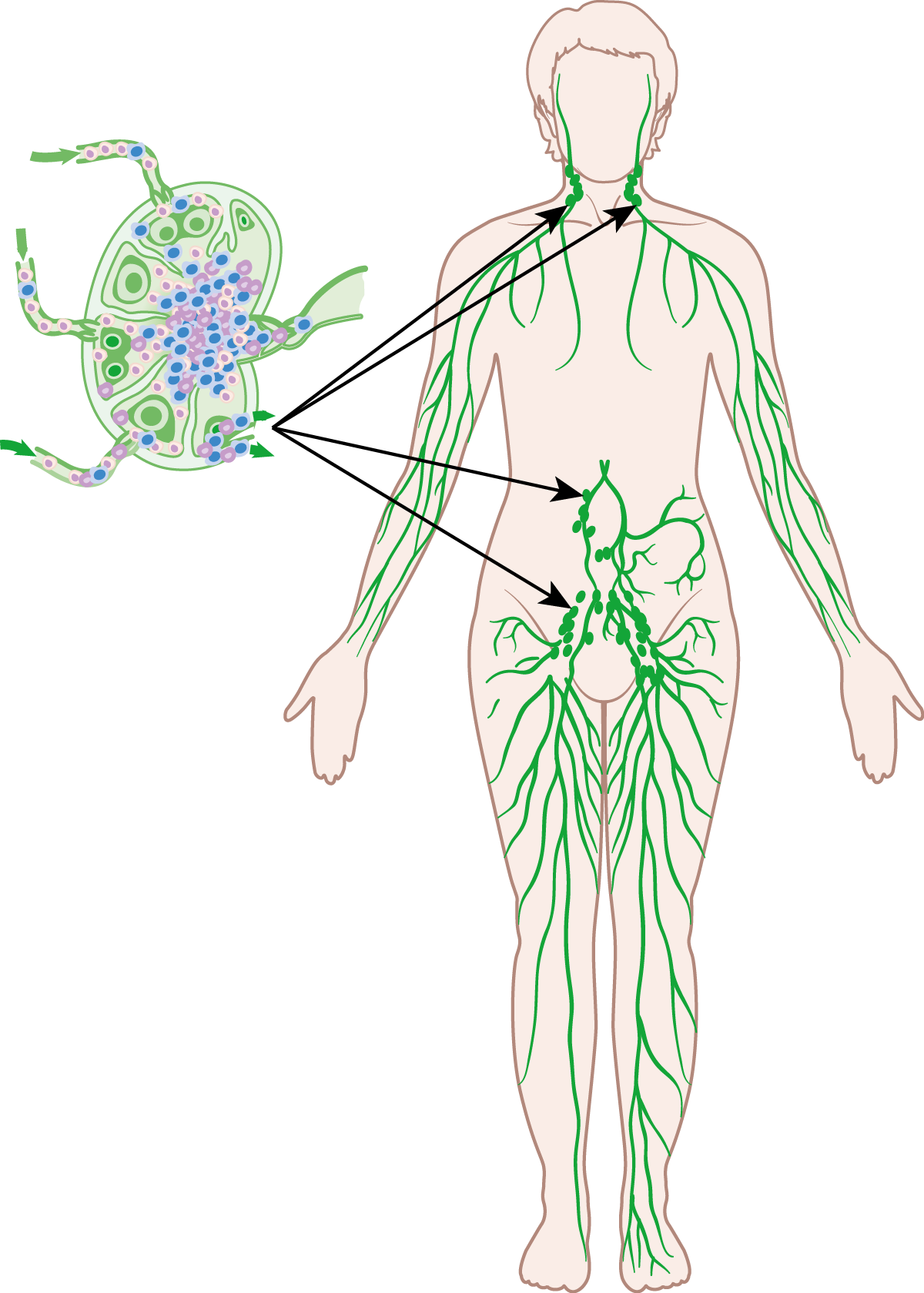
This information transfer, along with much of the action to follow, occurs within the lymphatic system, a network of vessels and nodes that drains and monitors the body’s fluids. Note that the connection between B and T cells and the lymphatic system is the source of the name given to both types of cells: lymphoctyes.
Lymph vessels form junctions at lymph nodes. Lymph nodes are the kidney shaped structures in the diagram on the right. Think of them as a type of organic filter that checks the body’s fluids for pathogens. As we’ll see below, the lymph nodes are where much of the action involved in the specific immune response occurs.
3. Phagocytes present antigen to helper T cells
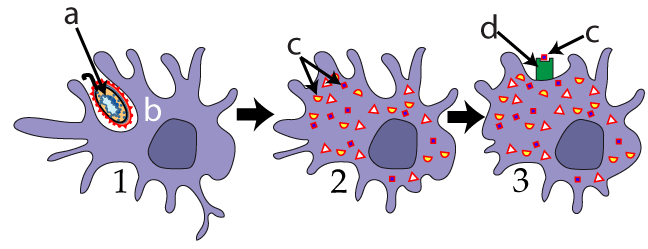
 Use the images at left to follow the action. Imagine these Helper T cells waiting in lymph nodes. When antigen presenting cell (“b”) arrives, it will use its Class II MHC protein (“d”) to present its antigen (“c”) to the waiting Helper T cells (one of which is shown at “e”). This presentation is completely tactile. If the shape of the presented antigen doesn’t complement the shape of the T cell receptor, then another helper T cell will come along and “attempt” to bind (there’s no intention, of course, which is why I added the quotes).
Use the images at left to follow the action. Imagine these Helper T cells waiting in lymph nodes. When antigen presenting cell (“b”) arrives, it will use its Class II MHC protein (“d”) to present its antigen (“c”) to the waiting Helper T cells (one of which is shown at “e”). This presentation is completely tactile. If the shape of the presented antigen doesn’t complement the shape of the T cell receptor, then another helper T cell will come along and “attempt” to bind (there’s no intention, of course, which is why I added the quotes).
But when the shapes complement each other (as shown in image 4, above), a weak intermolecular bond will form, keeping the helper T attached to the antigen presenting cell long enough for the helper T to grab on with an accessory protein called CD4 (shown at “g” in image 5). Once the APC and helper T are firmly in contact, the cells will secrete chemical messages, shown at “h” in image 6.
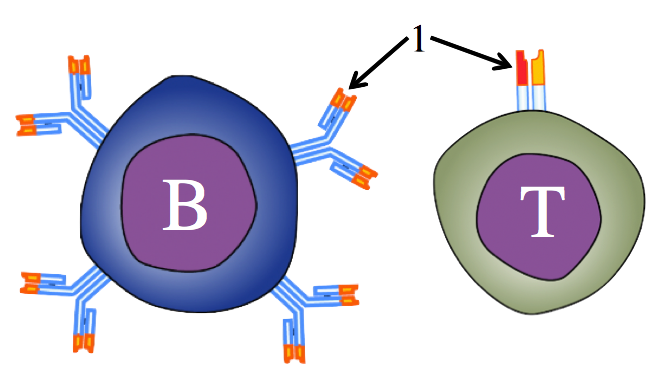
Many of these messages are cytokines. Cytokines have a variety of functions, but if you recognize a similarity between cytokine and cytokinesis, you’ve honed in on an important clue as to what cytokines do. These cytokines will induce cell division in the helper T cell. The result: many clones of the stimulated helper T, each one with a receptor for the antigen that was presented by the phagocyte in steps 1 through 6 above.
4. Helper T cells activate B cells, which become antibody-secreting Plasma Cells
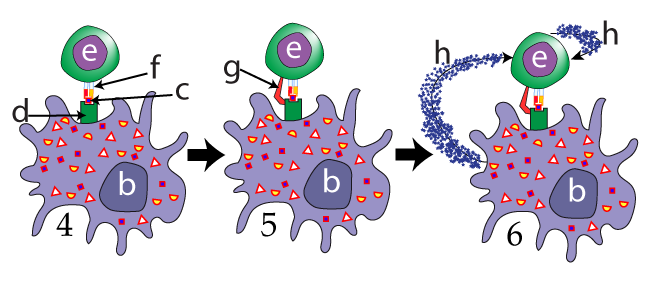
Note that, at this point, the immune system still hasn’t unleashed a response. But don’t worry: your infected finger is about to get some relief. There are now millions of cloned and activated helper T cells, each with a receptor for an antigen, waiting in a lymph node. What are they waiting for?
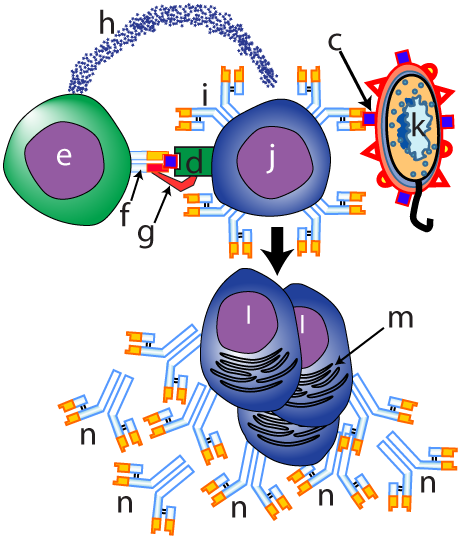 They’re waiting for a B cell (at letter “j” in the top-center of the image to your left) that has independently encountered the same pathogen (“k”). B cells are also phagocytic, and, like the phagocytic cell that started the recognition process, the B cell is displaying the antigen (represented by “c”) on its MHC class II protein (“d”). The key thing to notice here is the specificity involved in every step of this process. This B cell was only able to bind with the pathogen because it had a receptor (“i”) whose shape was complementary to the shape of a particular antigen on the invading pathogen. Similarly, the Helper T cell (“e”) is only able to bind to this B cell because its T cell receptor (“f”) is also complementary to the same antigen.
They’re waiting for a B cell (at letter “j” in the top-center of the image to your left) that has independently encountered the same pathogen (“k”). B cells are also phagocytic, and, like the phagocytic cell that started the recognition process, the B cell is displaying the antigen (represented by “c”) on its MHC class II protein (“d”). The key thing to notice here is the specificity involved in every step of this process. This B cell was only able to bind with the pathogen because it had a receptor (“i”) whose shape was complementary to the shape of a particular antigen on the invading pathogen. Similarly, the Helper T cell (“e”) is only able to bind to this B cell because its T cell receptor (“f”) is also complementary to the same antigen.
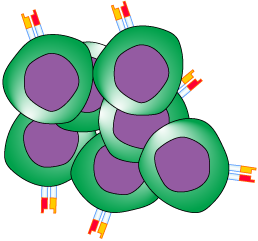
In a way that parallels the Helper T’s interaction with other antigen presenting cells, the Helper T will grab on to the B cell’s MHC protein with its CD4 protein (“g”). Locked together, the Helper T will release cytokines (“h”). These cytokines induce the B cell to differentiate into a clone of plasma cells (“i”).
The plasma cells are essentially antibody factories. Because antibodies are proteins that are destined for export for the cells, they’re made in the cell’s endoplasmic reticulum, represented by letter “m.” The goal of the process is shown at “n:” antibodies with an antigen binding site that complements the shape of specific antigen on an invading pathogen.Over the next few days following maturation, plasma cells will secrete up to 2000 antibodies/second/cell. But what do these antibodies do? Let’s review the sequence of events that got us to this point, and then we’ll see.
5. Interactive Table: The Humoral Response
[qwiz qrecord_id=”sciencemusicvideosMeister1961-Humoral Response, Interactive Table (Immune Sys.)”]
[h]Interactive Table: The Humoral Response
[i]
[q]The next card shows 10 of the steps of the humoral response, with some information missing. Drag words to make each step complete.
[q]
- _____________ engulfs a pathogen
- Phagocyte _________ the pathogen
- Phagocyte becomes an APC as it displays antigen on its_____ protein
- In a lymph node, a Helper T cell with a ______________ T cell receptor binds with displayed antigen
- Helper T and antigen presenting cell exchange_____________
- Helper T___________ itself into a swarm of identical, activated helper T cells
- An activated Helper T binds with a ________ displaying the original antigen
- Helper T cell releases ____________ that induce B cell cloning and ____________.
- B cell becomes a swarm of _______ cells
- Plasma cells release __________ that can bind with the antigen.
[l]antibodies
[fx] No. Please try again.
[f*] Excellent!
[l]B cell
[fx] No. Please try again.
[f*] Good!
[l]clones
[fx] No. Please try again.
[f*] Correct!
[l]complementary
[fx] No. Please try again.
[f*] Excellent!
[l]cytokines
[fx] No, that’s not correct. Please try again.
[f*] Great!
[l]differentiation
[fx] No, that’s not correct. Please try again.
[f*] Correct!
[l]digests
[fx] No. Please try again.
[f*] Correct!
[l]MHC
[fx] No, that’s not correct. Please try again.
[f*] Great!
[l]Phagocyte
[fx] No, that’s not correct. Please try again.
[f*] Correct!
[l]plasma
[fx] No, that’s not correct. Please try again.
[f*] Correct!
[x][restart]
[/qwiz]
6. Antibodies help neutralize pathogens in a variety of ways
Antibodies don’t directly destroy pathogens, but facilitate their destruction by other immune system components. Below, we’ll look at three ways in which antibodies work.
a. Neutralization of Viruses
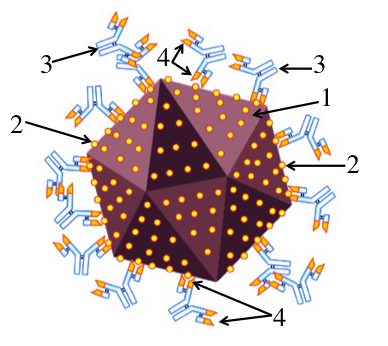
To neutralize is “to counteract the activity of: to make ineffective.” Merriam Webster. That’s what antibodies do to viruses. You can see that in this image (which we looked at in a previous tutorial). By binding with surface proteins (2) on a virus (1), antibodies (3) block viruses from binding with the membranes of the cells that they parasitize. Again, notice the specificity of the interaction. If the antigen binding site of the antibody (4) didn’t precisely complement the shape of the viral antigen, then the antibody wouldn’t bind to the virus.
b. Opsonization
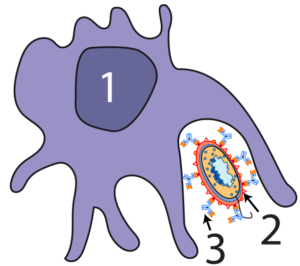
By binding with surface molecules on bacterial pathogens (2), antibodies (3) mark bacteria for attack by phagocytes (1).
c. Working with the Complement System
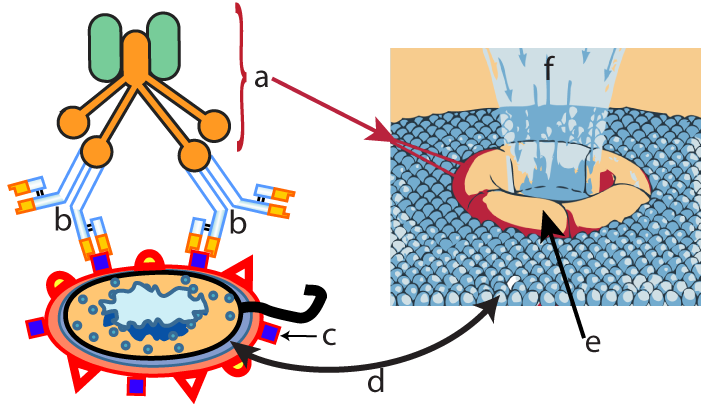
Complement (briefly discussed in my tutorial on non-specific immunity) consists of a team of proteins which can independently attack the membranes of invading cells. With the addition of antibodies, complement becomes even more effective. When antibodies (b) bind to antigens (c) on a pathogen’s membrane (d), the proteins in the complement system (a) become activated. These complement proteins form a membrane attack complex (e) that creates a hole in the membrane of the invading bacterial cell. Water and ions enter through these holes, causing the invader to burst from osmotic pressure.
7. The Humoral Response: Checking Understanding
[qwiz use_dataset=”SMV_humoral response” dataset_intro=”false” random = “true” qrecord_id=”sciencemusicvideosMeister1961-Humoral Response, CFU (Immune Sys.)”]
[h]The Humoral Response
[i]
[x]
[restart]
[/qwiz]
8. Next Steps
- Cell Mediated Immunity and Immunological Memory (the next tutorial in this series)
- Immune system main menu